INTRODUCTION
Telehealth has become a vital healthcare delivery model, especially in Sub-Saharan Africa, where geographic and infrastructure challenges limit care access. It provides immediate healthcare services and fosters economic, social, and human development by enhancing healthcare efficiency and reducing the time and costs associated with in-person consultations.1 Telehealth is particularly important for addressing healthcare disparities, promoting social equity, and bridging gaps between urban and rural areas. Its potential as a transformative tool for inclusive growth aligns with the broader goals in Information and Communication Technologies for Development (ICT4D).2,3
The COVID-19 pandemic accelerated the global adoption of telehealth, demonstrating its ability to address critical gaps when traditional healthcare systems are overwhelmed. However, Sub-Saharan Africa faces unique challenges, including limited internet access, unreliable electricity, and a scarcity of digital devices.4,5 Despite these obstacles, telehealth can significantly improve maternal health, chronic disease management, and mental health services. By facilitating access to specialized care in remote areas, telehealth can alleviate pressure on healthcare systems and enhance resilience in underserved communities.6,7
A significant barrier to telehealth implementation in Sub-Saharan Africa is the disparity in digital infrastructure. The Africa Information Society Initiative (AISI), launched in the 1990s, aimed to bridge these divides but often fell short due to its top-down approach and policy limitations.8 Reliable internet and broadband access are essential for real-time data exchange and telehealth services, yet rural areas often lack the connectivity needed. High mobile data costs can also exclude vulnerable populations from accessing crucial healthcare services.9 Addressing these systemic challenges could pave the way for more equitable healthcare solutions.
The digital gender gap also requires attention to ensure that telehealth is accessible to all community members. Women, often primary caregivers, typically have less access to technology, exacerbating healthcare disparities. Evidence from rural South Africa shows that increased ICT access can improve essential services such as healthcare, education, and sanitation.10 As digital access becomes increasingly vital for healthcare availability, bridging the gender technology gap is essential to ensure everyone can benefit from telehealth advancements. This study aims to answer the following questions: How to do disparities in digital infrastructure, like broadband penetration and mobile data affordability, impact telehealth implementation in Sub-Saharan Africa? This study uses secondary data analysis to evaluate telehealth readiness by examining key factors, including internet connectivity, broadband access, mobile data costs, rural connectivity, and the digital gender gap. By comparing these elements across different regions, the study aims to identify the challenges that hinder telehealth adoption and propose strategies to address them, ultimately promoting more equitable access to healthcare.
METHOD
Secondary Data Sources
This study utilizes the 2023 Digital Infrastructure in Africa report published by the Economic Commission for Africa (ECA). It comprehensively analyzes digital infrastructure across the continent and its role in enabling digital trade.11 Digital trade, which includes digitally enabled transactions of goods and services, has been recognized by the African Union Assembly of Heads of State and Government as a driver of socioeconomic transformation, prompting the inclusion of a Protocol on E-Commerce in the African Continental Free Trade Area (AfCFTA) Agreement.11 The report draws on data from credible organizations, such as the International Telecommunication Union (ITU) and the Groupe Speciale Mobile Association (GSMA), ensuring methodological rigor and reliability. It highlights key components of digital infrastructure essential for telehealth readiness, including broadband networks, internet exchange points (IXPs), data centers, and postal logistics.11 The report also emphasizes disparities in broadband penetration, rural-urban connectivity, affordability of internet services, and gender-based digital gaps, offering valuable regional breakdowns that align closely with the objectives of this study. We selected this report for its credibility and scope. It reflects the African Union’s Digital Transformation Strategy for 2020–2030, which identifies robust digital infrastructure as critical for driving digital inclusion and addressing systemic barriers to telehealth implementation,
Data Collection
Data collection involved a structured process of extracting telehealth-relevant variables from the ECA report. Key metrics included broadband network coverage (3G, 4G, and fixed broadband), mobile data affordability (calculated as the cost of 1GB of data as a percentage of Gross National Income), and the digital gender gap (the proportion of internet users disaggregated by gender). We selected these metrics based on their established importance in the literature for assessing digital infrastructure’s role in telehealth implementation. We use Excel in the extraction process to systematically organize the data and calculate summary statistics such as means, medians, and ranges for comparative analysis. To facilitate meaningful comparisons, we categorized data by region (North Africa, East Africa, West Africa, and Southern Africa). We also operationalized each metric by defining its measurement criteria. For example, broadband coverage was quantified as the percentage of the population with access to 3G or 4G networks. Additionally, we cross-referenced affordability indices with international benchmarks, such as those provided by the Broadband Commission, to contextualize the findings.
Measures
Several variables were identified to evaluate telehealth readiness comprehensively, including internet connectivity, broadband penetration, digital device affordability, and indicators of the digital divide. Internet connectivity was assessed based on the availability of 3G and 4G networks in each region. Broadband penetration was defined as the percentage of the population using mobile and fixed broadband services, focusing on rural-urban disparities. Digital device affordability was measured by the cost of entry-level smartphones and the Price of 1GB of mobile data as a percentage of gross national income (GNI). Telehealth readiness was assessed by examining the infrastructural capacity for digital health services, which factored in broadband and mobile network availability in rural and urban areas. The digital divide was analyzed by investigating gender-based disparities and rural-urban access differences, both critical for understanding equitable access to telehealth. Table 2 provides an overview of the criteria used for each variable.
Data Analysis
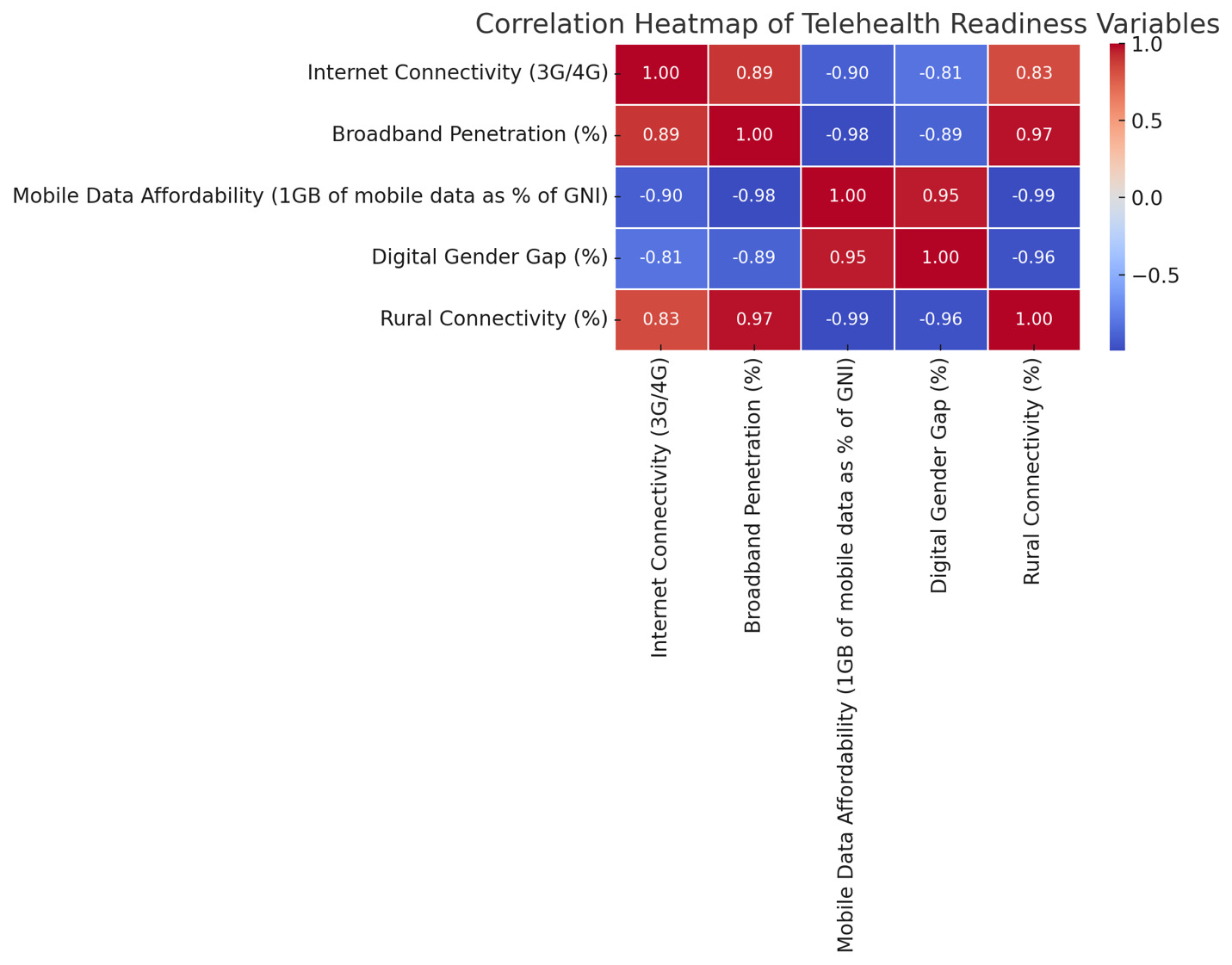
We used descriptive, comparative, and correlational techniques to evaluate telehealth readiness across African regions. Descriptive analysis summarized key metrics, such as broadband penetration, affordability, and rural-urban connectivity, using central tendency measures like means and medians. These summaries provided an initial understanding of disparities within and between regions. Comparative analysis highlighted differences between regions, such as North Africa’s higher broadband penetration than Sub-Saharan Africa. This analysis relied on regional averages and visual representations, such as bar charts, generated using Excel to illustrate these disparities. The correlational analysis explored the interdependencies among key variables, such as broadband penetration, mobile data affordability, and gender disparities, using Pearson’s correlation coefficient (r) to quantify these relationships. Steps to calculate Pearson’s correlation included normalizing variables to ensure comparability and applying standard correlation formulas. To enhance transparency, the analysis’s assumptions and limitations were explicitly addressed. For instance, while the data provided reliable insights, the study acknowledges that secondary data may not fully capture nuances such as localized socioeconomic or cultural barriers to telehealth adoption.
RESULTS
The analysis of telehealth readiness across different African regions, as reported in the Digital Infrastructure in Africa report, shows significant disparities that significantly affect development outcomes (see Figure 1). North Africa excels in several areas, such as broadband penetration (16.8%), mobile data affordability (2.5% of GNI), and rural connectivity (30%). This positions the region favorably for adopting telehealth services. Additionally, North Africa has a relatively low digital gender gap (20%), which suggests more equitable access to digital resources, particularly benefiting women who are often primary caregivers and may depend on telehealth for vital health services.
In contrast, West Africa, while boasting robust internet connectivity (70%), faces challenges with higher mobile data costs (8% of GNI) and a notable digital gender gap (30%). These issues could limit telehealth access in underserved communities. Southern Africa shows moderate internet connectivity (65%) and broadband penetration (8%) but struggles with high mobile data costs (7% of GNI) and a digital gender gap of 25%. East Africa experiences the most significant infrastructural challenges, marked by the lowest broadband penetration (5%), limited rural connectivity (10%), and the highest digital gender gap (40%). These challenges severely hinder equitable access to digital healthcare services. Figure 1 illustrates these regional disparities, showcasing North Africa’s advantages in digital infrastructure while highlighting East Africa’s significant obstacles to telehealth implementation.
Based on the Digital Infrastructure in Africa report, a comparative analysis between North and Sub-Saharan Africa further emphasizes these developmental challenges (see Figure 2). North Africa consistently outperforms Sub-Saharan Africa in critical indicators such as internet connectivity, broadband penetration, and mobile data affordability. With an average internet connectivity rate of 80% and lower mobile data costs (2.5% of GNI), North Africa benefits from substantial investments in digital infrastructure, making telehealth a more feasible and accessible option. In contrast, Sub-Saharan Africa wrestles with higher mobile data costs (8.3% of GNI) and lower broadband penetration (6.3%), along with limited rural connectivity (16.8%), all of which present significant barriers to telehealth adoption. Figure 2 visually contrasts these metrics, highlighting the stark differences in telehealth readiness between the two regions. These infrastructural limitations restrict access to telehealth services in rural and underserved areas, thereby obstructing efforts to improve healthcare equity and economic resilience.
Moreover, the digital gender gap represents a critical obstacle to achieving social equity in digital healthcare access. North Africa’s lower digital gender gap (20%) compared to the average of 31.2% in Sub-Saharan Africa highlights how gender disparities impact telehealth adoption. More equitable digital access for women in North Africa could foster overall health improvements and community development. In contrast, the higher gender gaps in Sub-Saharan Africa may limit healthcare access for women, adversely affecting maternal and child health outcomes and stifling human development potential. Hence, addressing these gender disparities is essential for unlocking telehealth’s full potential in promoting social and economic equity.
The correlational analysis emphasizes the interdependence of telehealth readiness factors within the IT for Development framework (see Figure 3). Internet connectivity (3G/4G) shows a strong positive correlation with broadband penetration (r = 0.89) and rural connectivity (r = 0.83), indicating that investments in broadband infrastructure boost connectivity in remote areas, thereby improving access to rural healthcare and support economic and human development. Conversely, internet connectivity negatively correlates with mobile data affordability (r = -0.90) and the digital gender gap (r = -0.81), suggesting that enhanced connectivity leads to more affordable digital services and promotes more significant gender equity. Figure 3 illustrates these correlation patterns, highlighting essential relationships between key telehealth readiness factors. Additionally, broadband penetration positively correlates with rural connectivity (r = 0.97), reinforcing the importance of broadband investments in expanding healthcare services in underserved regions.
DISCUSSION
The findings highlight the potential of targeted investments in broadband infrastructure to overcome multiple barriers to healthcare access. By enhancing rural connectivity, reducing mobile data costs, and addressing the digital gender gap, these investments can significantly improve telehealth readiness. This, in turn, would increase healthcare access, promote social inclusion, and stimulate economic growth. The strong negative correlation between mobile data affordability and rural connectivity (r = -0.99) underscores the urgent need to make digital services more affordable to extend telehealth access in rural and remote areas.
Addressing Gaps in Existing Literature
This study bridges critical gaps in the literature on telehealth and digital health in Sub-Saharan Africa by offering a granular analysis of regional disparities in digital infrastructure. The detailed examination of broadband penetration, mobile data affordability, and rural connectivity underscores the uneven distribution of digital resources. With broadband penetration at 16.8% and mobile data costs averaging 2.5% of GNI, North Africa benefits from relatively advanced infrastructure. At the same time, Sub-Saharan Africa lags significantly, with broadband penetration at 6.3% and data costs at 8.3% of GNI. These disparities, often underexplored in global digital health discussions, highlight their substantial implications for equitable healthcare access.
Additionally, this study reveals significant differences between mobile and fixed broadband penetration. Mobile broadband dominates in most Sub-Saharan regions due to its affordability and ease of deployment, particularly in rural and underserved areas.6 In contrast, fixed broadband, concentrated in urban centers, provides greater bandwidth and reliability but has significantly lower penetration rates, averaging 10% in many areas. This shows the reliance on mobile broadband as the primary driver of telehealth readiness in Sub-Saharan Africa while emphasizing the need for long-term investment in fixed broadband to support advanced healthcare applications.
Socioeconomic and Cultural Barriers
Socioeconomic and cultural barriers further complicate telehealth adoption in Sub-Saharan Africa. High poverty rates in rural areas limit the affordability of digital devices and mobile data plans, creating a significant obstacle to accessing telehealth services.9,11 Moreover, cultural factors such as mistrust of telehealth, preference for face-to-face consultations, and low digital literacy hinder widespread acceptance of these technologies.8,10 Traditional gender roles exacerbate these challenges, as women in many communities face restrictions on technology use and healthcare access, further widening the digital gender gap.2,6 For example, women in Sub-Saharan Africa are 31.2% less likely than men to use mobile internet, with the disparity being most pronounced in East Africa. Addressing these barriers requires targeted interventions that combine infrastructure investment with education and community engagement to promote digital inclusion.
Comparison with Global Standards and Initiatives
The findings are contextualized within global benchmarks and success stories, offering a comparative lens to evaluate telehealth readiness in Sub-Saharan Africa. Globally, Southeast Asia and Latin America have demonstrated innovative strategies for expanding internet accessibility. For instance, public-private partnerships in India successfully extended rural broadband coverage,16, while community Wi-Fi initiatives in Latin America, funded by non-profits, have bridged connectivity gaps.10 Similarly, Asia’s rapid adoption of telehealth during the COVID-19 pandemic was driven by high mobile broadband penetration rates, enabling cost-effective access to digital healthcare services.4,9 In contrast, Sub-Saharan Africa’s telehealth landscape remains limited due to network instability and constrained bandwidth. Europe’s reliance on fixed broadband for high-quality telehealth services, such as real-time video consultations and remote surgeries, highlights the importance of a balanced investment strategy.6,7 Sub-Saharan Africa can adopt lessons from these global successes by focusing on complementary mobile and fixed broadband investments to address its unique challenges. Aligning regional strategies with international initiatives, such as the World Health Organization’s digital health framework, can accelerate the development of equitable telehealth systems.
Theoretical Implications
This study contributes to broader theoretical frameworks on healthcare equity and digital health access. The strong correlation between broadband penetration and rural connectivity (r = 0.97) reinforces theories emphasizing digital infrastructure as a cornerstone for reducing health disparities. Improved connectivity directly correlates with enhanced healthcare access, particularly in resource-constrained settings, highlighting the critical role of infrastructure investment. The findings also deepen theoretical insights into the interplay between affordability, connectivity, and social inclusion. The strong negative correlation between mobile data affordability and the digital gender gap (r = -0.81) illustrates how reducing costs can promote equity in digital health access. Addressing the systemic barriers women face, such as social norms and economic constraints, is essential for unlocking telehealth’s potential to promote social justice. These insights advance the theoretical understanding of telehealth as a tool for addressing broader socioeconomic inequalities.
Infrastructural and Policy Implications
This study highlights the urgency of targeted investments in digital infrastructure to enhance telehealth readiness in Sub-Saharan Africa. Expanding broadband networks, reducing mobile data costs, and adopting gender-sensitive policies are critical to achieving equitable healthcare access. Policymakers must recognize the complementary roles of mobile and fixed broadband in driving telehealth adoption. With its widespread availability, mobile broadband should remain a priority for expanding connectivity in underserved rural areas.6,9 However, fixed broadband must also be developed to support high-bandwidth telehealth applications, particularly in urban centers where advanced digital health solutions can be piloted and scaled.
Furthermore, strategies from other regions provide actionable insights for addressing these challenges. Subsidized broadband for rural areas, incentives for telecommunications companies to invest in underserved regions, and gender-inclusive digital literacy campaigns targeting women can help bridge the digital divide. Stakeholder collaboration, including governments, private sector actors, NGOs, and international donors, drives infrastructure investment and promotes digital literacy.6,8 Practical steps such as pilot programs for mobile telehealth services in rural areas and targeted funding for gender-inclusive internet access projects can accelerate progress toward equitable healthcare systems.
CONCLUSION
This study highlights significant disparities and opportunities in telehealth implementation across Sub-Saharan Africa. While North Africa benefits from better digital infrastructure, lower mobile data costs, and more equitable access to technology for women, Sub-Saharan Africa faces significant challenges such as limited broadband access, high data costs, and a substantial digital gender gap. These findings contribute to the IT for Development literature by emphasizing how gaps in infrastructure hinder telehealth’s potential in resource-limited settings, which affects healthcare access and social equity. For practitioners, policymakers, technology providers, and healthcare professionals, the study emphasizes the necessity for targeted investments in broadband, policies to lower mobile data costs, and gender-sensitive strategies to bridge the digital divide. Addressing these issues is crucial to unlocking telehealth’s potential for promoting equitable healthcare access, reducing health disparities, and supporting sustainable development in underserved regions.